The Rising Threat of HIV: Why It’s Becoming a Dangerous Issue
- The Rising Threat of HIV: Why It’s Becoming a Dangerous Issue
- Introduction
- Let’s delve into the HIV infection rates. Here are some key facts:
- HIV stigma and discrimination are significant challenges faced by people living with HIV. Let’s explore this topic:
- Let’s explore the importance of early diagnosis and antiretroviral therapy (ART) in managing HIV:
- Lack of awareness and education indeed plays a significant role in the spread of HIV. Let’s explore this issue:
- HIV/AIDS has had a profound impact on global health. Let’s explore some key facts:
The Rising Threat of HIV: Why It’s Becoming a Dangerous Issue
Introduction
Human Immunodeficiency Virus (HIV) has been a persistent global health concern for several decades. Despite significant progress in prevention, diagnosis, and treatment, the virus continues to pose a dangerous threat to individuals, communities, and public health systems worldwide. Let’s explore why HIV remains a critical issue and the factors contributing to its resurgence.
Let’s delve into the HIV infection rates. Here are some key facts:
- Overall Trends in the United States:
- In the United States, estimated HIV infections decreased by 12% from 2017 to 2021.
- In 2021, approximately 32,100 new HIV infections occurred in the U.S. This represents a decline from 36,500 infections in 2017.
- The highest rates of new HIV diagnoses continue to occur in the Southern states.
- Transmission Categories:
- Men who have sex with men (MSM) accounted for 70% of the estimated new HIV infections in 2021 and 86% of infections among all males.
- People who acquired HIV through heterosexual contact accounted for 22% of the new infections in 2021. Among them, men reporting heterosexual contact accounted for 6%, while women reporting heterosexual contact accounted for 16% of estimated new HIV infections.
- People who inject drugs (PWID) accounted for 8% of the new infections in 2021.
- Demographic Disparities:
- Racial and ethnic minorities continue to be disproportionately affected by HIV. For instance, Black/African American individuals accounted for a significant proportion of new infections.
- Hispanic/Latino individuals also had a higher HIV prevalence rate compared to their population size.
- Global Context:
- Globally, an estimated 39.0 million people were living with HIV at the end of 2022, with 1.3 million new HIV infections occurring in that year.

image credit pinterest
HIV stigma and discrimination are significant challenges faced by people living with HIV. Let’s explore this topic:
- What is HIV Stigma?
- HIV stigma refers to negative beliefs and attitudes directed toward people with HIV. It often leads to labeling and discrimination against those living with the virus.
- Examples of HIV stigma include:
- Misconceptions: Believing that only certain groups or lifestyles lead to HIV transmission.
- Judgment: Assuming that people “deserve” HIV due to their life choices.
- Avoidance: Treating individuals differently because of their HIV status.
- Verbal Abuse: Using derogatory language to refer to people with HIV.
- HIV Discrimination:
- Discrimination encompasses the behaviors resulting from stigma. It includes:
- Healthcare Refusal: Some medical professionals may refuse care or services to people with HIV.
- Social Rejection: Casual contact avoidance due to HIV status.
- Derogatory Language: Harmful terms like “HIV-ers” or “positives.”
- Legal and Policy Restrictions: Criminal laws, travel bans, and employment limitations.
- Discrimination encompasses the behaviors resulting from stigma. It includes:
- Impact and Data:
- HIV stigma and discrimination:
- Affect Mental Health: People internalize stigma, leading to negative self-image.
- Reduce Access: Fear of discrimination discourages testing and seeking services.
- Violate Rights: Denial of employment, education, and health services.
- Data shows:
- Up to 21% of people with HIV report being denied healthcare.
- 40% faced forced medical procedures in some countries.
- Intersectional Discrimination: Race, disability, and socioeconomic status intersect with HIV stigma.
- HIV stigma and discrimination:
- Human Rights Perspective:
- HIV-related discrimination is a human rights issue.
- Everyone deserves dignity, protection, and access to rights regardless of their HIV status.
- Awareness and education can combat stigma, emphasizing community support and understanding.

image credit pinterest
Let’s explore the importance of early diagnosis and antiretroviral therapy (ART) in managing HIV:
- Early Diagnosis:
- Timely Testing: Early detection of HIV is crucial. Regular testing helps identify the virus even before symptoms appear.
- Benefits:
- Health Outcomes: Early treatment improves overall health and quality of life.
- Reduced Transmission: People on ART are less likely to transmit HIV to others.
- Prevent Complications: Early intervention prevents opportunistic infections.
- Antiretroviral Therapy (ART):
- ART involves taking a combination of medications to suppress HIV replication.
- How It Works:
- Viral Load Suppression: ART reduces the viral load (amount of virus in the blood) to undetectable levels.
- Immune System Support: It helps maintain a strong immune system.
- Long-Term Management: ART is a lifelong commitment.
- Benefits of ART:
- Prolongs Life: People on ART can live long, healthy lives.
- Reduces Transmission Risk: It reduces the risk.
- Prevents Opportunistic Infections: ART lowers the risk of infections like pneumonia, tuberculosis, etc.
- Preserves Immune Function: It prevents immune system decline.
- Challenges:
- Adherence: Taking medications consistently is essential for ART success.
- Side Effects: Some people experience side effects, but they can be managed.
- Access and Stigma: Ensuring access to ART and combating stigma are critical.
- Global Efforts:
- UNAIDS 90-90-90 Targets:
- By 2020: 90% of people living with HIV know their status.
- By 2020: 90% of diagnosed individuals receive ART.
- By 2020: 90% of those on ART achieve viral suppression.
- Ending AIDS: Early diagnosis and ART are key to achieving this goal.
- UNAIDS 90-90-90 Targets:
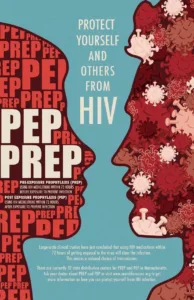
image credit pinterest
Lack of awareness and education indeed plays a significant role in the spread of HIV. Let’s explore this issue:
- Public Awareness:
- Misconceptions: Lack of accurate information leads to misconceptions about HIV transmission. People may believe that casual contact or sharing utensils can spread the virus.
- Stigma: Ignorance perpetuates stigma, making it harder for people to seek testing and treatment.
- Prevention: Awareness campaigns can educate the public about prevention methods like condom use, needle exchange programs, and PrEP (pre-exposure prophylaxis).
- Education:
- Schools and Communities: Comprehensive sex education in schools is crucial. Community programs can also raise awareness.
- Health Literacy: Understanding HIV risk factors, testing, and treatment options empowers individuals.
- Myths vs. Facts: Dispelling myths through education reduces stigma.
- Challenges:
- Taboos: Cultural and societal taboos hinder open discussions about sexual health.
- Access: Lack of access to education and healthcare exacerbates the problem.
- Language Barriers: Information must be available in diverse languages.
- Global Efforts:
- World AIDS Day: December 1st is dedicated to raising awareness about HIV/AIDS.
- UNAIDS: Global initiatives aim to end AIDS by 2030 through education, testing, and treatment.

image credit pinterest
HIV/AIDS has had a profound impact on global health. Let’s explore some key facts:
- Global Burden:
- HIV remains a major public health issue, having claimed approximately 40.4 million lives worldwide so far.
- Ongoing transmission occurs in all countries globally, with some reporting increasing trends in new infections even after previous declines.
- In 2022, approximately 630,000 people died from HIV-related causes, and 1.3 million people acquired HIV.
- Regional Distribution:
- WHO African Region: Two-thirds of people living with HIV (25.6 million) reside in this region.
- Leading Cause of Death: Particularly in Sub-Saharan Africa, HIV/AIDS is the leading cause of death.
- Chronic Condition Management:
- While there is no cure for HIV infection, access to effective prevention, diagnosis, treatment, and care has transformed HIV into a manageable chronic health condition.
- Antiretroviral therapy (ART) enables people living with HIV to lead long and healthy lives.
- Global Strategies:
- WHO, the Global Fund, and UNAIDS align their strategies with the Sustainable Development Goal (SDG) target 3.3 of ending the HIV epidemic by 2030.
- By 2025, the goal is for 95% of all people living with HIV to have a diagnosis, receive ART, and achieve a suppressed viral load.
WHO regional data:
African Region
- An estimated 25.6 million [21.6–30.0 million] people were living with HIV in 2022, of which 90% [76 to >98%] knew their status, 82% [69–96%] were receiving treatment and 76% [64–89%] had suppressed viral loads. An estimated 20.9 million people were receiving antiretroviral therapy in 2022.
- An estimated 660 000 [480 000–920 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages decreased to 0.57 [0.41–0.8] per 1000 uninfected population in 2022 from 1.75 [1.24–2.44] in 2010.
- 380 000 [300 000–540 000] deaths were attributed to HIV-related causes in 2022, a decrease of 56% from 2010.
Region of the Americas
- An estimated 3.8 million [3.4–4.3 million] people were living with HIV in 2022, of which 86% [76–97%] knew their status, 71% [62–79%] were receiving treatment and 65% [57–73%] had suppressed viral loads. An estimated 2.7 million people were receiving antiretroviral therapy in 2022.
- An estimated 160 000 [130 000–190 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages decreased to 0.16 [0.13–0.19] per 1000 uninfected population in 2022 from 0.18 [0.15–0.21] in 2010.
- 41 000 [31 000–54 000] deaths were attributed to HIV-related causes in 2022, a decrease of 37% from 2010.
South-East Asian Region
- An estimated 3.9 million [3.4–4.6 million] people were living with HIV in 2022, of which 81% [70–94%] knew their status, 65% [57–76%] were receiving treatment and 61% [53–71%] had suppressed viral loads. An estimated 2.6 million people were receiving antiretroviral therapy in 2022.
- An estimated 110 000 [85 000–160 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages decreased to 0.06 [0.04–0.08] per 1000 uninfected population in 2022 from 0.12 [0.09–0.16] in 2010.
- 85 000 [62 000–120 000] deaths were attributed to HIV-related causes in 2022, a decrease of 63.4% from 2010.
European Region
- An estimated 3.0 million [2.6–3.3 million] people were living with HIV in 2022, of which 72% [64–80%] knew their status, 63% [55–70%] were receiving treatment and 60% [53–67%] had suppressed viral loads. An estimated 1.9 million people were receiving antiretroviral therapy in 2022.
- An estimated 180 000 [150 000–220 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages increased to 0.20 [0.16–0.23] per 1000 uninfected population in 2022, from 0.16 [0.13–0.18] in 2010.
- 52 000 [40 000–65 000] deaths were attributed to HIV-related causes in 2022, an increase of 36.9% from 2010.

Eastern Mediterranean Region
- An estimated 490 000 [420 000–600 000] people were living with HIV in 2022, of which 38% [33–47%] knew their status, 27% [23–33%] were receiving treatment and 24% [21–29%] had suppressed viral loads. An estimated 130 000 people were receiving antiretroviral therapy in 2022.
- An estimated 56 000 [47 000–76 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages decreased to 0.07 [0.06–0.1] per 1000 uninfected population in 2022 from 0.05 [0.04–0.06] in 2010.
- 20 000 [16 000–27 000] deaths were attributed to HIV-related causes in 2022, an increase of 72.3% from 2010.
Western Pacific Region
- An estimated 2.2 million [1.7–2.8 million] people were living with HIV in 2022, of which 81% [60 to >98%] knew their status, 73% [55–91%] were receiving treatment and 70% [53–88%] had suppressed viral loads. An estimated 1.6 million people were receiving antiretroviral therapy in 2022.
- An estimated 140 000 [100 000–190 000] people acquired HIV in 2022; and the number of people acquiring HIV among all ages remained stable at 0.07 [0.05–0.1] per 1000 uninfected population in 2022 from 0.07 [0.05–0.09] in 2010.
- 51 000 [30 000–80 000] deaths were attributed to HIV-related causes in 2022, a decrease of 24.7% from 2010 but an increase of 3.5% compared with 2021.
Promoting safe sexual practices in cities is essential for public health and well-being. Here are some strategies that cities can adopt:
- Education and Awareness:
- Comprehensive Sex Education: Implement sex education programs in schools and community centers. Educate people about safe sex practices, contraception, and sexually transmitted infections (STIs).
- Campaigns: Run public awareness campaigns on safe sex, condom use, and regular STI testing.
- Accessible Healthcare Services:
- Clinics and Testing Centers: Ensure easy access to STI testing, counseling, and treatment centers.
- Contraceptive Services: Provide affordable and confidential contraceptive services.
- Safe Public Spaces:
- Lighting and Surveillance: Well-lit streets and surveillance cameras discourage illicit activities and promote safety.
- Design Considerations: Urban planning can create safe spaces for everyone, including women and LGBTQ+ individuals.
4)Community Engagement:
-
- Engage Grassroots Organizations: Collaborate with local NGOs, community groups, and women’s organizations to raise awareness and provide support.
- Peer Educators: Train peer educators to disseminate information about safe sex practices.
5)Legal Framework:
-
-
- Anti-Discrimination Laws: Enforce laws that protect against discrimination based on sexual orientation and gender identity.
- Sexual Harassment Laws: Strictly enforce laws against sexual harassment in public spaces.
-
6)Inclusivity and Diversity:
-
-
-
- LGBTQ+ Inclusion: Create safe spaces for LGBTQ+ individuals. Address their unique needs and challenges.
- Cultural Sensitivity: Understand diverse cultural norms related to sexuality and adapt strategies accordingly.
-
-
7)Collaboration with Stakeholders:
-
-
-
-
- Government Agencies: Work with health departments, police, and social services.
- Businesses and Entertainment Venues: Encourage responsible practices in nightlife areas.
-
-
-
More You can visit: https://taazakhobor.in/
More you can read:
How alcohol can harm your body? best blog of 2024. Don’t miss at all
Crypto Airdrops in 2024: All the important things
How to look young and beautiful and handsome naturally in 2024. No harmful process
How brain works psychology. 99% people don’t know
Why sleep is important for health? The topic that 99.99% people don’t even know!!